KINSHASA et LUMUMBASHI, le 7 octobre 2025 (La Fondation Apprendre Genève) – « Ces jeunes filles qui ont des grossesses indésirables, quand elles mettent au monde, elles ont tendance à laisser les enfants livrés à eux-mêmes », explique Marguerite Bosita, coordonnatrice d’une organisation non gouvernementale à Kinshasa.
« Ce manque d’informations sur les questions liées à la vaccination se pose encore plus, car ces enfants grandissent exposés à des difficultés de santé ».
Sa voix, émanant d’une mission de terrain dans la province du Kongo Central, s’est jointe à des centaines d’autres ce 7 octobre 2025.
Il s’agissait de la deuxième journée d’un exercice d’apprentissage par les pairs de 16 jours visant à identifier et à atteindre les enfants dits « zéro dose » en République démocratique du Congo (RDC).
Ce sont ces centaines de milliers de nourrissons qui n’ont reçu aucun vaccin pour les protéger de nombreuses maladies.
Pour les 1 617 professionnels de la santé inscrits à cet exercice, il ne s’agissait pas d’un webinaire de formation classique, mais d’une étape importante d’un mouvement bien plus large.
Organisé par La Fondation Apprendre Genève, cet exercice est une pierre angulaire du Mouvement congolais pour la vaccination à l’horizon 2030 (IA2030).
Il bénéficie du soutien du ministère de la Santé de la RDC à travers son Programme élargi de vaccination (PEV), de l’UNICEF et de Gavi, l’Alliance du Vaccin.
L’initiative renverse le modèle traditionnel de l’aide internationale.
Au lieu de s’appuyer sur des experts extérieurs, elle part d’un postulat aussi simple qu’il est conséquent.
La meilleure expertise pour résoudre les défis de première ligne se trouve chez les travailleurs de la santé eux-mêmes.
La composition de cette cohorte témoigne de la profondeur de l’initiative.
Plus de la moitié des participants proviennent des niveaux périphériques et infranationaux du système de santé, là où la vaccination a lieu.
Un professionnel sur cinq travaille au niveau central, assurant un lien essentiel entre les politiques nationales et les réalités du terrain.
Le profil des participants est tout aussi varié.
Un tiers sont des médecins, 30 % des agents de santé publique, suivis par les agents de santé communautaire (13 %) et les infirmiers (9 %).
Fait marquant, près de la moitié d’entre eux travaillent directement pour le ministère de la Santé à travers le Programme élargi de vaccination (le «PEV»).
Cette forte proportion de personnel gouvernemental, complétée par une représentation significative de la société civile et du secteur privé, ancre fermement l’initiative dans une appropriation nationale.
Le regard du terrain
« Les défis sont tellement grandioses », a déclaré Franck Kabongo, consultant en santé publique à Lubumbashi, dans la province du Haut-Katanga.
En effet, les défis décrits par les participants sont immenses.
Il a souligné deux obstacles majeurs.
D’une part, la difficulté d’atteindre les enfants dans les communautés reculées.
Car les problèmes logistiques représentent un « casse-tête» pour de nombreux acteurs de santé impliqué dans la vaccination.
Pour Mme Bosita à Kinshasa, le problème est profondément social.
Son organisation soutient les enfants vulnérables, y compris les orphelins et ceux qui vivent dans la rue, dont beaucoup sont nés de jeunes mères sans suivi médical.
« Il n’y a pas assez de sensibilisation sur le terrain par rapport à cette notion », a-t-elle déploré, expliquant sa volonté d’intégrer la vaccination dans le travail de son association.
Ces témoignages, partagés dès les premières minutes, ont brossé un tableau saisissant d’un corps de métier dévoué.
Ils luttent contre un enchevêtrement complexe de barrières logistiques, sociales et informationnelles qui laissent les enfants les plus vulnérables sans protection.
À la recherche des causes profondes
Le cœur de l’exercice n’est pas seulement de partager les problèmes, mais de les disséquer.
Grâce à une analyse de groupe structurée, les participants s’exercent à la technique des « cinq pourquoi ».
Cette méthode vise à dépasser les symptômes pour trouver la véritable cause fondamentale d’un problème.
Lors d’une session plénière, Charles Bawande, animateur communautaire dans la zone de santé de Kalamu à Kinshasa, a présenté un dilemme courant.
Une forte concentration d’enfants zéro dose parmi les communautés de rue, très mobiles et souvent peu scolarisées.
Au départ, le problème semblait être un simple manque d’information.
Mais au fur et à mesure que le groupe a creusé, une réalité plus complexe est apparue.
Pourquoi les enfants sont-ils manqués?
Parce que les travailleurs de santé communautaires, les relais communautaires, ne disposent pas des informations nécessaires.
Pourquoi n’ont-ils pas ces informations?
Parce qu’ils n’assistent souvent pas aux séances d’information essentielles.
Pourquoi n’y assistent-ils pas?
Parce qu’ils sont occupés par d’autres activités.
« Ils doivent vivre, ils doivent manger… ils sont locataires, ils doivent payer le loyer », a expliqué M. Bawande.
La dernière question a révélé le cœur du problème.
Pourquoi sont-ils occupés par d’autres choses?
Parce que leur travail de relais communautaire est entièrement bénévole.
Alors qu’on attend d’eux qu’ils agissent comme des volontaires, beaucoup sont des parents et des chefs de famille qui doivent donner la priorité à leur gagne-pain.
Un problème qui semblait être un simple déficit d’information s’est révélé être ancré dans la précarité économique du système de santé bénévole.
Une mosaïque de défis partagés
Lorsque les participants se sont répartis en près de 80 petits groupes, leurs discussions ont révélé un large éventail d’obstacles, chacun profondément lié au contexte local.
Les rapports des groupes ont dressé une carte riche et détaillée des freins à la vaccination à travers le vaste pays.
Près de Goma, dans le Nord-Kivu, le groupe de Clémence Mitongo a identifié l’insécurité due à la guerre comme une barrière principale qui a déplacé les populations et perturbé les services de santé.
Dans la province du Kasaï, le groupe de Yondo Kabonga a mis en lumière l’impact des rumeurs, de la désinformation et des barrières géographiques comme les ravins et les rivières.
Ailleurs, d’autres groupes ont fait état de la résistance issue de convictions religieuses, certaines églises enseignant à leurs fidèles que la foi seule suffit à protéger leurs enfants.
Un autre groupe a discuté du cas des réfugiés revenus d’Angola, où l’ignorance des parents concernant le calendrier vaccinal constitue un obstacle majeur.
Ce diagnostic collectif a démontré la puissance du modèle d’apprentissage par les pairs.
Aucun expert ne pourrait à lui seul posséder une compréhension aussi fine et étendue des défis à l’échelle nationale.
Une nouvelle façon d’apprendre
Cet exercice est fondamentalement différent des programmes de formation traditionnels.
Il s’agit d’un parcours pratique où les participants deviennent des créateurs de connaissances et leaders des actions qui en découlent.
Au cours du programme, chaque participant développera son propre projet de terrain, qu’il partagera avec son équipe, son centre de santé ou son district.
Il s’agit d’un plan concret pour s’attaquer à un défi « zéro dose » dans sa propre communauté.
Après avoir soumis une version préliminaire d’ici le vendredi 10 octobre, ils entreront dans une phase d’évaluation par les pairs.
Chaque participant recevra les retours de trois collègues et, en retour, en fournira à trois autres, contribuant ainsi à renforcer le travail de chacun par l’intelligence collective.
Tracer une voie à suivre
L’étape suivante pour ces milliers de professionnels de la santé est de consolider leurs discussions de groupe et de poursuivre le travail sur leurs projets individuels avant l’échéance de vendredi.
Le parcours se poursuivra avec des phases consacrées à l’évaluation par les pairs, à la révision des projets et, enfin, à une assemblée générale de clôture pour partager les plans améliorés.
Cet exercice intensif est plus qu’un simple événement.
Il est un catalyseur pour le Mouvement congolais pour la vaccination à l’horizon 2030.
L’objectif est de traduire la stratégie mondiale du Programme pour la vaccination à l’horizon 2030 en actions tangibles, menées localement, qui produisent un impact réel.
La solution, comme le suggère ce mouvement, ne se trouve pas dans des lignes directrices venues de Genève, mais dans la sagesse, la créativité et l’engagement combinés de milliers de praticiens congolais, travaillant ensemble à travers tout le pays.
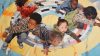
Illustration: The Geneva Learning Foundation Collection © 2025